Abstract

Introduction
In traditional analysis of cancer clinical trials, key endpoints such as progression-free survival (PFS) and overall survival (OS) are often analysed separately. Using multistate models (MSMs) we can model these events simultaneously to holistically analyse the disease-treatment pathway. This provides meaningful estimates for the probability of disease progression and death at any point in the disease course, incorporating treatment and prognostic factors of interest. MSMs are also a useful tool to assess the relationship between how the time spent in one state affects the risk of transitioning to future states. In the context of myeloma (MM), this can be used to determine patient prognosis based on the time for which they remain in 1 st remission after initial treatment.
Methods
In the largest randomised trial of MM patients undertaken to date (NCRI Myeloma XI), newly diagnosed MM patients eligible for ASCT (NDMM TE) were randomised to induction, intensification and maintenance treatments. Maintenance randomisation, at ASCT+3 months, was to lenalidomide (R), lenalidomide plus vorinostat (RZ) or observation. Co-primary endpoints were PFS and OS analysed by Cox regression.
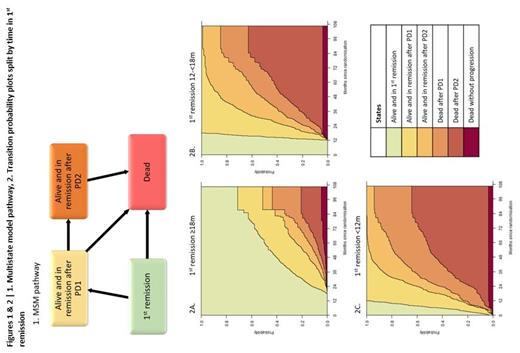
An MSM was used for exploratory analysis of 1074 TE patients randomised to maintenance. Patients transitioned irreversibly between 4 states: 1 st remission, alive and in remission after 1 st progressive disease (PD1), alive and in remission after 2 nd PD (PD2) and dead (Figure 1). Time in 1 st remission was included as a covariate to assess the effect of early disease progression on subsequent state transitions (<12 months n=172, 12-18m n=106, ≥18m n=796).
Results
The median follow-up from randomisation was 57m (interquartile range: 43-72m). MSM analysis found that a 1 st remission of <12m from randomisation was associated with a highly increased risk of transition to PD2 following PD1 (hazard ratio (HR) 4.54, 95% confidence interval (CI) 3.20-6.43) and death (HR 1.93, 95%CI 1.17-3.20) vs. a 1 st remission of ≥18m. A 1 st remission of 12-18m was also associated with an increased risk of transition to PD2 following PD1 (HR 2.79, 95%CI 1.96-3.96), but was not associated with an increased risk of death following PD1 (HR 0.95, 95%CI 0.61-1.47) vs. a 1 st remission of ≥18m.
At a snapshot at 5 years post-randomisation, those with a 1 st remission ≥18m had a 24.9% chance of being in the PD1 state, compared to just 6.4% and 1.1% in those with 1 st remissions of 12-18m and <12m respectively (Figure 2). Furthermore, this group had a 6.1% chance of death following PD1 and 5.7% chance of death following PD2. In those with a 1 st remission of 12-18m, this increased to 31.0% and 38.8%, and in those <12m to 29.3% and 48.6%, respectively.
MSM analysis also found R and RZ were associated with a reduced risk of transition from 1 st remission to PD1 vs. observation (R HR 0.51, 95%CI 0.42-0.60; RZ HR 0.68, 95%CI 0.55-0.88), reflecting the results of the primary trial analysis of PFS. Primary trial analysis of OS found that R was associated with significantly longer OS than observation. However, MSM analysis found R was associated with an increased risk of death following both PD1 (HR 1.60, 95%CI 1.06-2.41) and PD2 (HR 1.46, 95%CI 1.03-2.07) vs. observation. This suggests that the OS benefit of R is gained by extending the time in 1 st remission. RZ was associated with increased risk of death without PD (HR 3.07, 95%CI 1.05-9.03) and death following PD2 (HR 1.49, 95%CI 0.99-2.26) vs. observation. The MSM also found that the expected duration in 1 st remission was longest for R and shortest for observation (R 56.7m, RZ 47.7m and obs. 38.6m). However, in the PD1 state (R 12.8m, RZ 15.7m and obs. 21.9m) and PD2 state (R 5.4m, RZ 7.3m and obs. 11.0m) this order was reversed, although the difference between the groups was reduced for later states.
Discussion
MSMs are a powerful tool for exploring the myeloma disease pathway, identifying associations between states and providing transition probabilities which can be easily interpreted to gain further insights to those obtained via traditional methods. MSMs are an effective method to visualise data, clearly demonstrating the association between early relapse post-ASCT and poor prognosis in NDMM. This work has expanded on the primary analysis of the maintenance randomised treatments in Myeloma XI, corroborating results previously observed and highlighting the potential effects of maintenance treatment on each stage of the disease pathway.
Craig: Celgene: Research Funding; Merck Sharpe & Dohme: Research Funding; Amgen: Research Funding; Takeda: Research Funding. Pawlyn: Amgen: Honoraria; Janssen: Honoraria, Membership on an entity's Board of Directors or advisory committees; Sanofi: Honoraria, Membership on an entity's Board of Directors or advisory committees; Celgene / BMS: Honoraria, Membership on an entity's Board of Directors or advisory committees. Kaiser: AbbVie: Consultancy; BMS/Celgene: Consultancy, Other: Travel support, Research Funding; Janssen: Consultancy, Other: Educational support, Research Funding; GSK: Consultancy; Karyopharm: Consultancy, Research Funding; Takeda: Consultancy, Other: Educational support; Pfizer: Consultancy; Amgen: Honoraria; Seattle Genetics: Consultancy. Olivier: Celgene / BMS: Research Funding; Amgen: Research Funding; Takeda: Research Funding; Merck Sharpe and Dohme: Research Funding. Jones: Janssen: Honoraria; BMS/Celgene: Other: Conference fees. Drayson: Abingdon Health: Current holder of individual stocks in a privately-held company. Jenner: Takeda: Consultancy; Pfizer: Consultancy; Janssen: Consultancy, Honoraria, Speakers Bureau; BMS/Celgene: Consultancy, Honoraria, Speakers Bureau. Cook: Amgen: Consultancy; BMS/Celgene: Consultancy, Research Funding; Janssen: Consultancy, Research Funding; Takeda: Consultancy, Research Funding; Sanofi: Consultancy; Karyopharm: Consultancy. Davies: BMS: Consultancy, Honoraria; Amgen: Consultancy, Honoraria; Abbvie: Consultancy, Honoraria; Takeda: Consultancy, Honoraria; Roche: Consultancy, Honoraria; Janssen: Consultancy, Honoraria. Morgan: BMS: Membership on an entity's Board of Directors or advisory committees; Jansen: Membership on an entity's Board of Directors or advisory committees; Karyopharm: Membership on an entity's Board of Directors or advisory committees; Oncopeptides: Membership on an entity's Board of Directors or advisory committees; GSK: Membership on an entity's Board of Directors or advisory committees. Jackson: J and J: Consultancy, Honoraria, Speakers Bureau; GSK: Consultancy, Honoraria, Speakers Bureau; takeda: Consultancy, Honoraria, Research Funding, Speakers Bureau; amgen: Consultancy, Honoraria, Speakers Bureau; celgene BMS: Consultancy, Honoraria, Research Funding, Speakers Bureau; oncopeptides: Consultancy; Sanofi: Honoraria, Speakers Bureau. Cairns: Celgene / BMS: Other: travel support, Research Funding; Merck Sharpe and Dohme: Research Funding; Amgen: Research Funding; Takeda: Research Funding.
Author notes
 This icon denotes a clinically relevant abstract
This icon denotes a clinically relevant abstract